Urinary Tract Infection (UTI)
Urinary incontinence (UI) is an extremely common complaint in every part of the world and in any century! It causes a great deal of distress and embarrassment, as well as significant costs, to both individuals and societies. Estimates of prevalence vary according to the definition of incontinence and the population studied. However, there is universal agreement about the importance of the problem in terms of human suffering and economic cost.
Prevalence of Urinary Incontinence:
- The prevalence is 4.5% to 53% for women, 1.6% to 24% for men, the prevalence increases with age.
- The prevalence of neurogenic bladder disorder (with or without urinary incontinence) increases with age in women from 2% to 19% with a steep increase in women older than 44 years.
- In men, the prevalence is 1% to 9% with a steep increase in men older than 64 years.
- Urinary incontinence is also highly prevalent in the geriatric population. Successful care requires a strong working knowledge of fundamental geriatric principles.
Unfortunately, Only Few People Acknowledge Their Condition and Seek a Consultation to Solve the Problem.

The International Continence Society (ICS) defines urinary incontinence as “the complaint of any involuntary loss of urine”.
Classification and Causes of Urinary Incontinence
Stress Incontinence: it is urine leakage, which is associated with increased abdominal pressure and insufficient urethral sphincter mechanism. The main symptom of stress incontinence is the loss of urine on exertion, sneezing or coughing.
Stress urinary incontinence is mainly due to a lack of the pelvic floor support, so during strain there is an abnormal mobility of the pelvic floor organs, and especially of the urethra; what happens to pelvic organs in case of lack of support can be compared to a man on an hammock; when the support (the rope) breaks, the man falls down; this is how loss of urine happens during exercises.
Urge incontinence: it is defined as urinary incontinence due to active detrusor contractions. If a neurological disease is present, urge incontinence is also called detrusor hyperreflexia. The main symptom is involuntary urine loss together with urgency; this condition is called overactive bladder.

Giggle incontinence is a special form of urge incontinence (enuresis risoria): laughter triggers detrusor contractions and causes urge incontinence. Giggle incontinence is most common in children.
Mixed Urinary Incontinence: it is the combination of stress incontinence and urge incontinence.
Overflow Incontinence: in chronic urinary retention, urinary incontinence is caused by an increase of the bladder pressure without detrusor contractions, which exceeds the urinary sphincter pressure.
Extraurethral Urinary Incontinence: it is urine leakage via channels independent from the urethra: vesicovaginal fistula (mainly due to obstetric causes), urethrovaginal fistula or malformations such as ectopic ureter.
Diagnosis
The diagnosis of urinary incontinence can be done by physical examination and by urodynamic investigation; this is a sophisticated test that is done in the outpatient clinic, and is able to assess completely the bladder function (or dysfunction).
Treatment
Treatment for urinary incontinence depends on the type of incontinence, its severity and the underlying cause. A combination of treatments may be needed.
Doctors are likely to suggest the least invasive treatments first and move on to other options only if these techniques fail.
Behavioral techniques
it can be recommended:
Bladder training, to delay urination after you get the urge to go. You may start by trying to hold off for 10 minutes every time you feel an urge to urinate. The goal is to lengthen the time between trips to the toilet until you’re urinating only every 2.5 to 3.5 hours.
Double voiding, to help you learn to empty your bladder more completely to avoid overflow incontinence. Double voiding means urinating, then waiting a few minutes and trying again.
Scheduled toilet trips, to urinate every two to four hours rather than waiting for the need to go.
Fluid and diet management, to regain control of your bladder. You may need to cut back on or avoid alcohol, caffeine or acidic foods. Reducing liquid consumption, losing weight or increasing physical activity also can ease the problem.
Pelvic floor muscle exercises
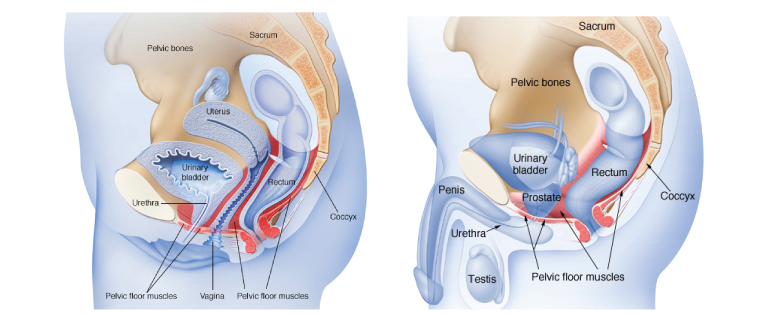
Female pelvic floor muscles Male pelvic floor muscles
Exercises aim to strengthen the muscles that help control urination; these are as Kegel exercises, and are especially effective for stress incontinence but may also help urge incontinence.
Electrical strimulation
Electrodes are temporarily inserted into rectum or vagina to stimulate and strengthen pelvic floor muscles; electrical stimulation can be effective for stress incontinence and urge incontinence.
Medications
Medications commonly used to treat incontinence include:
Anticholinergics. These medications can calm an overactive bladder and may be helpful for urge incontinence.
Mirabegron. Used to treat urge incontinence, this medication relaxes the bladder muscle and can increase the amount of urine your bladder can hold. It may also increase the amount of urine passing at one time, helping to empty bladder more completely.
Alpha blockers. In men with urge or overflow incontinence, these medications relax bladder neck muscles and muscle fibers in the prostate and make it easier to empty the bladder.
Topical estrogen. For women, applying low-dose, topical estrogen in the form of a vaginal cream, ring or patch may help tone and rejuvenate tissues in the urethra and vaginal areas. Systemic estrogen — taking the hormone as a pill — isn’t recommended for urinary incontinence and may even make it worse.
Medical devices
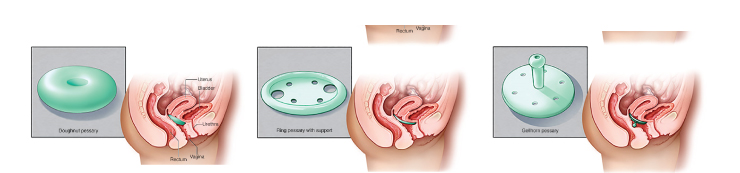
Devices designed to treat women with incontinence include mainly pessaries.
Interventional therapies that may help with incontinence include:
Bulking material injections A synthetic material is injected into tissue surrounding the urethra. The bulking material helps keep the urethra closed and reduce urine leakage. This procedure is generally much less effective than more-invasive treatments such as surgery for stress incontinence and usually needs to be repeated regularly.
Botulinum toxin type A (Botox) Injections of Botox into the bladder muscle may benefit people who have an overactive bladder. Botox is generally prescribed to people only if other first line medications haven’t been successful.
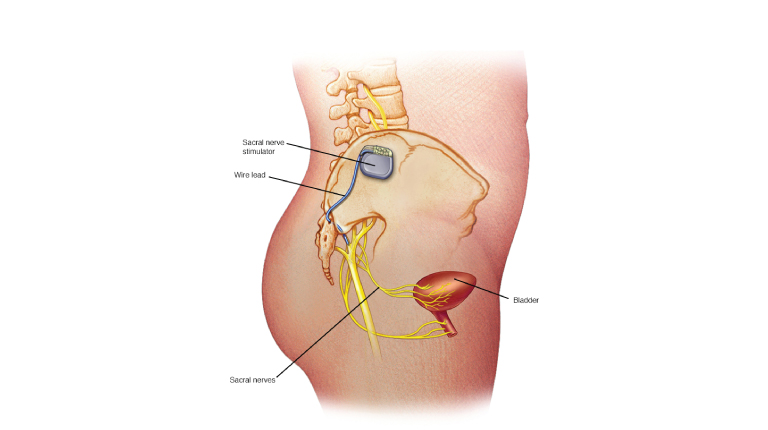
Sacral nerve stimulators
Sacral nerve stimulation device, it modulates the activity of the nerves that go to the bladder; it is mainly active on urge urinary incontinence (overactive bladder)
A device resembling a pacemaker is implanted under the skin to deliver painless electrical pulses to the nerves involved in bladder control (sacral nerves). Stimulating the sacral nerves can control urge incontinence if other therapies haven’t worked.
Surgery
If other treatments aren’t working, several surgical procedures can treat the problems that cause urinary incontinence:
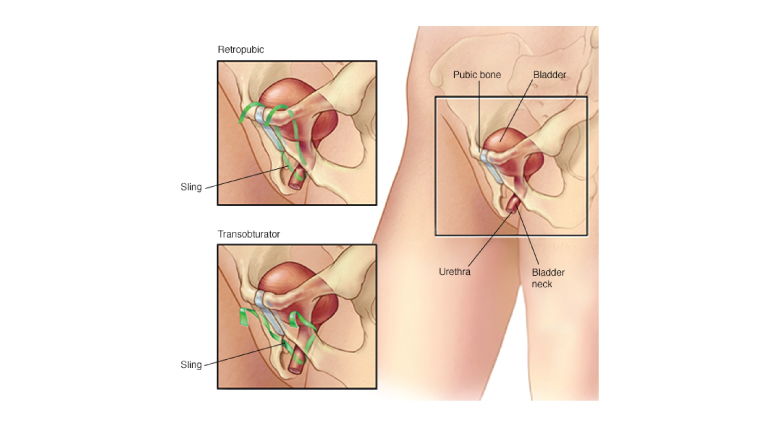
Sling procedures. Synthetic material or mesh are used to create a pelvic sling around your urethra. The sling helps keep the urethra closed, especially when you cough or sneeze. This procedure is used to treat stress incontinence.
Bladder neck suspension This procedure is designed to provide support to your urethra and bladder neck — an area of thickened muscle where the bladder connects to the urethra. It involves an abdominal incision, so it’s done during general or spinal anesthesia.
Prolapse surgery In women with mixed incontinence and pelvic organ prolapse, surgery may include a combination of a sling procedure and prolapse surgery.
Artificial urinary sphincter Mainly in men, but also in women, a small, fluid-filled ring is implanted around the urethra or the bladder neck to keep the urinary sphincter shut until you’re ready to urinate. To urinate, a valve implanted under skin can be pressed, causing the ring to deflate and allowing urine from the bladder to flow.






